Cancer of the Pancreas (Pancreatic Cancer): What to Know
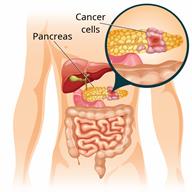
Pancreatic cancer is a type of cancer in which a cancerous (malignant) tumor develops in the pancreas. The pancreas is a gland in the abdomen between the stomach and the spine. The pancreas makes hormones and enzymes that help the body control blood sugar, digest food, and store energy from food.
There are two types of pancreatic cancer:- Exocrine. This is the most common type.
- Endocrine. This is also called islet cell cancer or pancreatic neuroendocrine tumor (NET).
Pancreatic cancer can spread (metastasize) to other parts of the body.
What are the causes?
The exact cause of this condition is not known.
What increases the risk?
The following factors may make you more likely to develop this condition:- Being over 65 years old.
- Smoking cigarettes.
- Having a family history of cancer of the pancreas, colon, or ovaries.
- Having diabetes.
- Having long-term inflammation of the pancreas (chronic pancreatitis).
- Being exposed to certain chemicals.
- Eating a diet that is high in fat and red meat.
What are the signs or symptoms?
In the early stages, there are often no symptoms of this condition. As the cancer gets worse, symptoms may vary depending on the type of pancreatic cancer you have. Common symptoms include:- Nausea and vomiting.
- Loss of appetite and weight loss.
- Pain in the upper abdomen or upper back.
- Skin or the white parts of the eyes turning yellow (jaundice).
- Fatigue.
- Itchy skin.
- Dark urine.
- Stools that are:
- Light-colored and greasy-looking.
- Black and tarry-looking.
- High blood sugar (hyperglycemia). This may cause increased thirst and frequent urination.
- Low blood sugar (hypoglycemia). This may cause confusion, sweating, and a fast heartbeat.
- Depression.
How is this diagnosed?
This condition may be diagnosed based on your medical history and a physical exam. Your health care provider may:- Check your skin and eyes for signs of jaundice.
- Check for excess fluid in the abdomen and changes in the abdomen near the pancreas.
- Do blood and urine tests, imaging tests, biopsy, and genetic testing.
- The size of the tumor.
- If the cancer has spread.
- Where the cancer has spread.
How is this treated?
Depending on the type and stage of your pancreatic cancer, treatment may include:- Surgery to remove all or part of the pancreas or to remove the tumor.
- If the cancer has spread, portions of the stomach, bile duct, spleen, and small intestine may also be removed.
- Chemotherapy. This uses medicine to destroy the cancer cells.
- Radiation therapy. This uses high-energy beams to kill cancer cells.
- Medicine to attack a tumor's genes and proteins (targeted therapy). These medicines may limit the damage to healthy cells.
- Participating in clinical trials to see if new (experimental) treatments are effective.
- Medicines to help manage pain and other symptoms.
A combination of surgery, radiation therapy, and chemotherapy may be used.
Follow these instructions at home:
Medicines
-
Take over-the-counter and prescription medicines only as told by your health care provider.
-
Ask your health care provider about changing or stopping your regular medicines. These include any diabetes medicines or blood thinners you take.
-
Do not take dietary supplements or herbal medicines unless your health care provider tells you to. Some supplements can interfere with how well the treatment works.
- Ask your health care provider if the medicine prescribed to you:
- Requires you to avoid driving or using machinery.
- Can cause constipation. You may need to take these actions to prevent or treat constipation:
- Drink enough fluid to keep your urine pale yellow.
- Take over-the-counter or prescription medicines.
- Eat foods that are high in fiber, such as beans, whole grains, and fresh fruits and vegetables.
- Limit foods that are high in fat and processed sugars, such as fried or sweet foods.
Lifestyle
-
Get enough sleep on a regular basis. Most adults need 6–8 hours of sleep each night. During treatment, you may need more sleep.
-
Rest as told by your health care provider.
-
Consider joining a cancer support group. Ask your health care provider about local and online support groups. This may help you to cope with the stress of having pancreatic cancer.
-
Do not use any products that contain nicotine or tobacco. These products include cigarettes, chewing tobacco, and vaping devices, such as e-cigarettes. If you need help quitting, ask your health care provider.
Eating and drinking
-
Try to eat regular, healthy meals. Some of your treatments might affect your appetite. If you are having problems eating, see a food and nutrition specialist (dietitian).
-
Do not drink alcohol.
General instructions
-
Work with your health care provider to manage any side effects of your treatment.
-
Return to your normal activities as told by your health care provider. Ask your health care provider what activities are safe for you.
-
Keep all follow-up visits. These monitor the treatments and guide next steps.
Where to find more information
-
American Cancer Society: www.cancer.org
-
National Cancer Institute (NCI): www.cancer.gov
Contact a health care provider if:
-
You have new or worsening abdominal pain or nausea.
-
You have diarrhea or a change in bowel movements.
-
You have swelling or redness anywhere, especially around a cut or wound.
-
You have pain or burning when urinating.
-
You cannot eat or drink without vomiting.
-
You have worsening or unexplained weight loss.
Get help right away if:
-
You have a fever.
-
Your pain suddenly gets worse.
-
You have trouble breathing.
-
You have chest pain or an irregular heartbeat.
-
You have blood in your vomit or dark, tarry stools.
-
You have bloating or pain in the abdomen.
-
Do not wait to see if the symptoms will go away.
-
Do not drive yourself to the hospital.
Summary
-
Pancreatic cancer is a tumor in the pancreas that is cancerous (malignant).
-
Risk factors include having a family history of cancer of the pancreas, colon, or ovaries.
-
Treatment may include surgery, chemotherapy, and radiation therapy.
-
Consider joining a cancer support group.
-
Keep all follow-up visits. These monitor the treatments and guide next steps.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.

