Clubfoot, Pediatric
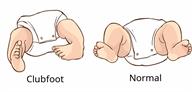
Clubfoot is a condition in which a child is born with one foot or both feet that turn inward (misshapen or deformed). The bottom of the foot may face sideways or even upward. In babies with clubfoot, a leg tendon is shorter and tighter than normal. This is why the foot turns inward. The twisting can range from mild to severe.
It is important to start treatment within 1-3 weeks after birth. After corrective bracing, a child may be able to walk, wear shoes, and play sports.
What are the causes?
The exact cause of this condition is not known.
What are the signs or symptoms?
 Symptoms of this condition include:
Symptoms of this condition include:- A foot that twists inward.
- A lower leg that looks short, small, or thin.
- A deep crease along the bottom of the foot.
How is this diagnosed?
Your child's health care provider can diagnose clubfoot:- With ultrasound imaging before birth.
- With a physical exam at the time of birth.
How is this treated?
The goal of treatment is to straighten the foot so your child can stand or walk painlessly with the sole of the foot flat on the ground. The foot shape can usually be corrected with stretching, casting, and bracing. In rare cases, surgery is needed. The treatment plan may include:- Gently stretching the foot toward the normal position.
- Holding the foot in place with a full leg cast. In some cases, taping may be used in place of casting.
- Removing the cast each week, stretching the foot toward the normal position, and then placing a new cast. This process is continued for 5 to 8 weeks or until the foot is in a normal position.
- Your child may need to wear a special brace (boots and bar brace) to prevent the deformity from coming back. This brace has both shoes attached to a bar. It keeps the foot in a normal position. Your child may need to wear this brace for several years. At first your child will wear this brace almost all the time. The time in the brace is gradually reduced after the first 3 months.
- In some cases, your child may require a procedure to correct the problem. If this is required, your child's health care provider:
- Will cut the strong tissue that connects the leg muscles to the heel (Achilles tendon) in order to release tension on the foot. This procedure involves a small cut near the heel but no stitches. If the tendon is cut, your child will need to wear a cast for several weeks until healed.
- Will perform other corrective surgery. This may be needed if the deformity is not completely corrected with stretching and bracing, or if the deformity returns after stretching and bracing.
- A health care provider who treats and corrects deformities of the bones, joints, and muscles (orthopedist).
- A brace specialist (orthotist).
- A physical therapist.
Follow these instructions at home:
If your child has a nonremovable cast:
-
Do not allow your child to put pressure on any part of the cast until it is fully hardened. This may take several hours.
-
Do not allow your child to stick anything inside the cast to scratch his or her skin. Doing that increases the risk of infection.
-
Check the skin around the cast every day. Tell your child's health care provider about any concerns.
-
You may put lotion on dry skin around the edges of the cast. Do not put lotion on the skin underneath the cast.
-
Keep the cast clean.
- If the cast is not waterproof:
- Do not let it get wet.
- Cover it with a watertight covering when your child takes a bath or a shower.
If your child has a brace:
-
Have your child wear the brace as told by your child's health care provider. Remove it only as told by your child's health care provider.
-
Loosen the brace if your child's toes become pale or turn cold and blue.
-
Keep the brace clean.
General instructions
-
After stretching and casting is over, make sure your child wears the brace as told by the health care provider.
-
Check your child's feet for blisters every day.
-
Keep all follow-up visits. This is important.
Where to find more information
-
American Academy of Orthopedic Surgeons: orthoinfo.aaos.org
Contact a health care provider if:
-
Your child has a fever.
-
Your child seems to be in pain.
-
Your child develops skin redness, irritation, or blisters from the cast or brace.
-
Your child has a brace, and the foot keeps coming out of the brace.
Get help right away if:
-
Your child who is younger than 3 months has a temperature of 100.4°F (38°C) or higher.
-
Your child's toes turn blue while in a cast.
Summary
-
Clubfoot is a deformity a child is born with.
-
Clubfoot is diagnosed at birth with a physical exam or during pregnancy with an ultrasound.
-
Treatment starts soon after birth to return the foot to a normal position for standing and walking.
-
Clubfoot usually responds to treatment that involves stretching and casting for several months, then wearing a brace for a few years.
-
In some cases, a procedure to correct the problem may be needed.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.

