Cancer of the Uterus (Uterine Cancer): What to Know
Uterine cancer is a disease in which cancer cells form and grow in the uterus. These cancer cells can also spread to other parts of the body.
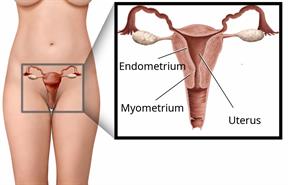
The wall of the uterus has an inner layer of tissue called the endometrium. It also has an outer layer of muscle tissue called the myometrium. The most common type of uterine cancer starts in the endometrium. Cancer that starts in the myometrium is very rare.
What are the causes?
The cause of this condition is not known.
What increases the risk?
You are more likely to get this cancer if:- You are over age 50.
- The lining of your uterus is thicker than normal. This is called endometrial hyperplasia.
- You or family members have had cancer of the uterus, colon, or ovary.
- You started your period before age 12. And you continue to have periods after age 52.
- You have never been pregnant.
- You have taken hormones to treat some conditions. Or you have taken a medicine called tamoxifen.
- You have had some conditions for a long time, such as diabetes, obesity, or polycystic ovary syndrome.
What are the signs or symptoms?
-
You have abnormal bleeding or discharge from the vagina. This includes spotting between periods or bleeding after menopause.
-
You lose weight without knowing why.
-
You have trouble peeing. You may also have pain when you pee, or you may pee too often.
- You may have big changes when you poop. For example:
- You may not poop enough.
- You may poop too often.
- Your poop may change color.
-
You have bloating or fullness in the belly.
-
You have pain in the belly or the pelvis. Or pain during sex.
How is this diagnosed?
This condition may be diagnosed based upon:- Your symptoms and medical history.
- A physical exam.
- Testing a piece of tissue from the uterus for abnormal cells (biopsy).
- Imaging, such as ultrasound, X-ray, CT scan, MRI, and PET scan.
- Blood and pee (urine) tests.
Your cancer will be staged. Staging checks how bad the cancer is and whether it has spread to other organs.
How is this treated?
Treatment for this condition depends on the type and stage of the cancer. It may include:- Surgery to remove the uterus and cervix (simple hysterectomy) or the uterus, cervix, fallopian tubes, and ovaries (total hysterectomy).
- Chemotherapy or targeted cell therapy. This uses medicines to kill cancer cells or to slow their growth.
- Radiation therapy. This uses high-energy rays to kill cancer cells and prevent their spread.
- Brachytherapy. This uses small radioactive capsules to kill any remaining cancer cells after surgery.
- Hormone therapy. This uses hormones or hormone-blocking medicines to fight cancer cells.
- Immunotherapy. This uses medicines to help your immune system fight cancer cells.
Follow these instructions at home:
Medicines
-
Take over-the-counter and prescription medicines only as told by your health care provider.
-
Work with your provider to manage the side effects of treatment.
General instructions
-
Do not smoke, vape, or use any products that have nicotine or tobacco. If you need help quitting, talk with your provider.
-
Do not have sex, douche, or place anything in your vagina until your provider says it's safe. Do not use tampons or diaphragms.
-
Eat a healthy diet. A healthy diet includes a lot of fruits and vegetables, low-fat dairy products, lean meats, and fiber.
-
Return to your normal activities as told by your provider. Ask your provider what activities are safe for you.
-
Keep all follow-up visits. Your care team will monitor your condition closely and may need to change your treatment.
Where to find support
Think about joining a support group for people who have been diagnosed with cancer.
Where to find more information
-
American Cancer Society: cancer.org
-
National Cancer Institute: cancer.gov
Contact a health care provider if:
-
You have a fever or chills.
-
You have pain in your pelvis or belly, and the pain gets worse.
-
You see big changes in your poop or the way you poop.
-
You see big changes in the way you pee.
-
You bleed from the vagina and it gets worse.
-
You have new symptoms that worry you.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.

