Diabetes During Pregnancy (Gestational Diabetes): What to Know
Gestational diabetes mellitus, or gestational diabetes, is diabetes that some people get when pregnant. This condition usually happens at 24–28 weeks of pregnancy.
People with gestational diabetes have high blood sugar. If you do not get treated for this condition, it may cause problems for you and your baby.
It goes away after you give birth but can happen again the next time you become pregnant.
What are the causes?
 This condition is caused by changes in your body when you're pregnant. When these changes happen:
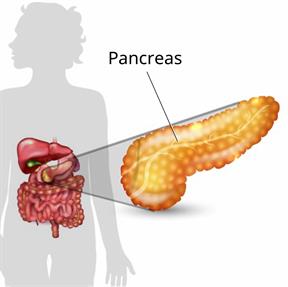
This condition is caused by changes in your body when you're pregnant. When these changes happen:- The pancreas may not make enough insulin.
- The body may not use insulin in the right way. This is called insulin resistance.
Insulin helps your body use sugar for energy. If your body doesn't have enough insulin or can't use the insulin that it has, extra sugars stay in your blood. This leads to high blood sugar (hyperglycemia).
What increases the risk?
-
Being older than age 25 when pregnant.
-
Too much body weight.
-
Having polycystic ovary syndrome (PCOS).
-
Having someone with diabetes in your family.
-
Having had this condition in the past.
-
Being pregnant with more than one baby.
What are the signs or symptoms?
You may not have any symptoms. If you do have symptoms, they may include:- Being thirsty often.
- Being hungry often.
- Needing to pee more often.
These symptoms can be missed because they're similar to other symptoms of pregnancy.
How is this diagnosed?
This condition may be diagnosed based on your blood sugar level and how your body responds to glucose. This may be checked with an oral glucose tolerance test (OGTT). The test may be done:- Early in pregnancy if you have risk factors.
- At 24–28 weeks of your pregnancy.
How is this treated?
To treat this condition, you may be told to:- Eat a healthy diet.
- Get more exercise.
- Check your blood sugar often.
- Your health care provider will tell you what your target is.
- Take insulin and other medicines. These are taken if needed.
- Work with a diabetes expert.
Follow these instructions at home:
Learn about your diabetes
Ask your provider:- How often should I check my blood sugar? Where do I get the equipment?
- What medicines do I need? When should I take them?
- Do I need to meet with an educator?
- Who can I call if I have questions?
- Where can I find a support group?
General instructions
- Take medicines only as told by your provider.
- Stay at a healthy weight.
- Drink enough fluid to keep your pee (urine) pale yellow.
- Check your pee for ketones when sick and as told.
- Ketones in your pee is a sign that your body is using fat for energy because it's not making enough insulin.
- Wear an alert bracelet or carry a card that shows you have this condition.
- Keep all follow-up visits. Your provider needs to check your health and your baby's growth.
Where to find more information
-
Gestational Diabetes: American Diabetes Association (ADA): diabetes.org
-
Gestational Diabetes and Pregnancy: Centers for Disease Control and Prevention (CDC): cdc.gov
-
American Pregnancy Association: americanpregnancy.org
-
U.S.D.A MyPlate: myplate.gov
Contact a health care provider if:
-
Your blood sugar is above your target for two tests in a row.
-
You have a high blood sugar level and you also have ketones in your pee.
-
You have been sick or have had a fever for 2 days or more and aren't getting better.
- You have any of these problems for more than 6 hours:
- You can't eat or drink.
- You vomit or feel like you may vomit.
- You have watery poop (diarrhea).
Get help right away if:
-
You become confused or cannot think clearly.
-
You have trouble breathing.
-
You have chest pain.
-
Your baby is moving less than usual.
-
You have unusual discharge or bleeding from your vagina.
-
You have cramping in your belly or have pain in your hips or lower back.
- You have symptoms of high blood pressure or preeclampsia. These include:
- A severe, throbbing headache that doesn't go away.
- Sudden or extreme swelling of your face, hands, legs, or feet.
- Vision problems, such as:
- Seeing spots.
- Blurry vision.
- Sensitivity to light.
-
Do not wait to see if the symptoms will go away.
-
Do not drive yourself to the hospital.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.

